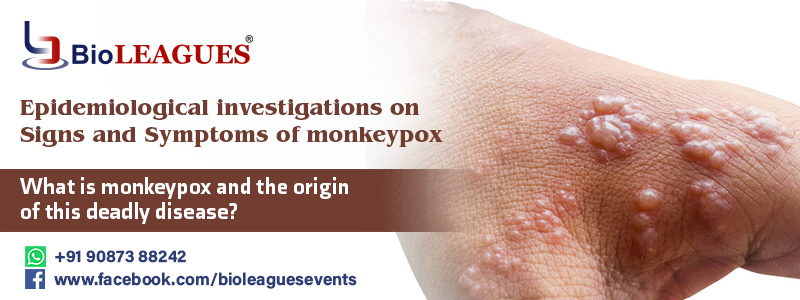
What is monkeypox and the origin of this deadly disease?
Monkeypox is a viral zoonotic disease (an infective virus transmitted from animals to humans) with signs that are comparable to those seen in patients in the past, however, it is less severe clinical. Monkeypox has been identified as the most vital orthopoxvirus for public health since the eradication of smallpox in 1980 and the consequent suspension of smallpox vaccination. Monkeypox is mostly seen in Central and West Africa, especially near deep tropical rainforests, and is becoming more common in wide urban areas. Animal hosts include rats and non-human mammals.
What are the study results of international medical conferences on monkeypox?
The importance of the Monkeypox virus, an enclosed double-stranded DNA virus that belongs to the Orthopoxvirus genus of the Poxviridae family, was highlighted in a recent medical conference’s valuable keynote sessions. Sessions with the two separate genetic clades of the monkeypox virus: the central African (Congo Basin) clade and the West African clade were held during the event. The Congo Basin clade was assumed to be more transmittable and caused more severe sickness in the past. It is the only country in which both viral clades have been detected; it has been divided geographically.
The Monkeypox virus’s natural hosts
- The monkeypox virus is vulnerable in a variety of animal species. The major symptoms of monkeypox are visible in Rope squirrels, tree squirrels, Gambian pouched rats, dormice, non-human primates, and other species.
- The Symptoms of monkeypox virus are still unknown, and further research is needed to determine the specific reservoir(s) and how virus circulation is sustained in nature.
The Unexpected Outbreak of Human Monkeypox
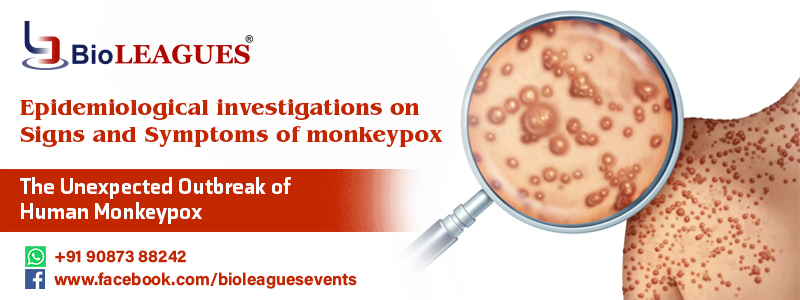
Human monkeypox was discovered early in a 10-month-old baby in the Democratic Republic of Congo in 1970, in an area where smallpox had been eradicated in 1968. Ever since, the majority of cases were reported from the Congo Basin’s rural, rainforest regions, mainly in the Democratic Republic of Congo, and human cases are reported from throughout central and West Africa.
Human cases of monkeypox have indeed been recorded in 11 African countries since 1970:
Monkeypox’s real burden has yet to be determined. In the Democratic Republic of Congo, an outbreak was recorded with a lower case fatality ratio and a greater attack rate than typical. A monkeypox outbreak was discovered at the same time, which explains the real or perceived changes in transmission dynamics in this instance. Nigeria has been dealing with a major outbreak since 2018, with over 400 infected patients, over 300 confirmed cases and a case fatality rate of over 3%. Cases are still being reported today.
We recognized a medical conference in 2003 using informative Conference alerts, where we discussed monkeypox outbreaks that occurred outside of Africa, in the United States of America and were associated with exposure to infected pet prairie dogs.
The animals were kept in cages with Gambian pouched rats and dormice that had been brought from Ghana. Over 60 cases of monkeypox were reported in the United States as a result of this outbreak. Tourists from Nigeria to Israel in October 2018, the U.k in November 2019, May 2021 and May 2022, Malaysia in May 2019, and the U.s.a. in July and November 2021 have all been documented to have monkeypox.
Various cases of monkeypox were discovered in many non-endemic countries in May 2022. Studies are now being conducted to learn more about the epidemiological, infection origins, and transmit patterns.
Major Signs and Symptoms of monkeypox
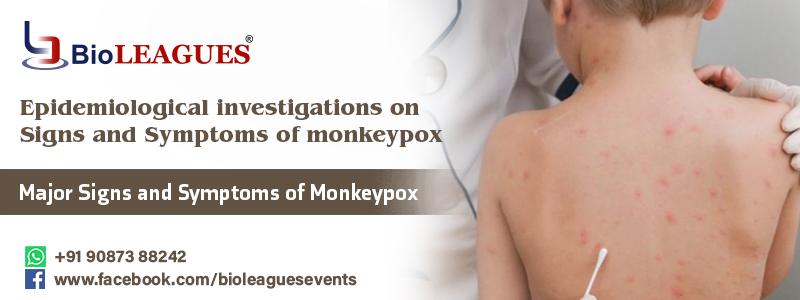
Monkeypox takes 4 to 12 days to incubate, although it can take anywhere from 6 to 22 days.
The infection is categorized into two:
These invasion periods are characterized by fever, intense headache, lymphadenopathy, back pain, myalgia, and intense asthenia. It is a distinctive feature of monkeypox compared to other diseases that may initially appear similar (chickenpox, measles, smallpox).
The skin eruption usually begins with the appearance of fever. It tends to be more concentrated on the face and extremities rather than on the trunk. It specifically targets the face (in 95% of cases), forearms of the hands, and toes (in 76 percent of cases). Oral mucous membranes (in 73 % of patients), genitalia (23 %), conjunctivae (16 %), and the cornea is also impacted. It evolves sequentially from macules (lesions with a flat base) to papules (slightly raised firm lesions), vesicles (lesions filled with clear fluid), pustules (lesions filled with yellowish fluid), and crusts that dry up and fall off. The quantity of lesions might range from a few to thousands. Lesions can brilliantly coalesce until big chunks of skin tear off in severe situations.
- Monkeypox is typically a self-limiting illness that lasts 3 to 5 weeks. Severe instances are more frequent in youngsters and are linked to the amount of virus exposure, the patient’s condition, and the type of problems. Autoimmune deficiencies may serve a role in the outcome.
- Monkeypox has a mortality rate that has traditionally fluctuated from 0% to 11% in the general population, with a greater rate among small children. In latest days, the case fatal crash ratio has hovered around 5–7%.
Conclusion:
When it concludes, it needs to end with the prevention, so the primary prevention strategy for monkeypox is to raise public knowledge of risk factors and educate individuals about the steps they may take to decrease their transmission of the virus. Presently, scholar research is being carried to the viability and adaptability of vaccination for monkeypox prevention and treatment.
Bioleagues is hosting a fantastic upcoming conference to promote awareness of monkeypox and provide vaccines to those who may be at risk, such as laboratory personnel, quick response teams, and health workers. Click to learn more about them.